Minde Strief
2018 Courage Ride Patient Honoree
Melinda’s Chondrosarcoma Journey
I am sharing my journey for Sarcoma Awareness Month to help support what University of Iowa Health Care does to continually make strides to find cures and improve lives, and to reach out to others around the world who need hope, advice, a shoulder to cry on, laughter to get them through the tough times.
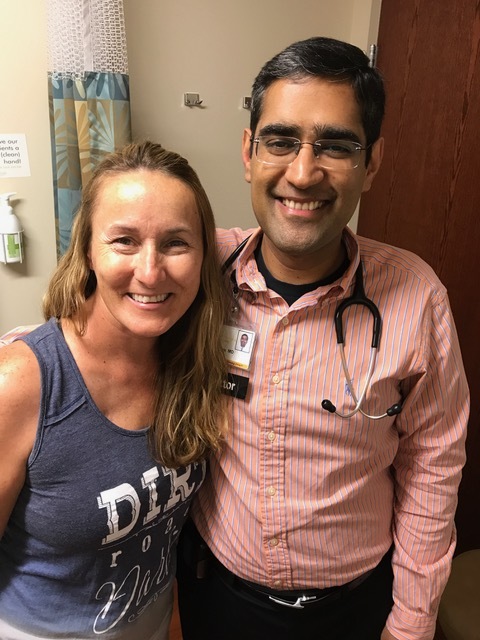
I put my trust, faith, and body into the hands of two strangers, two highly recommended doctors—Benjamin Miller and Mohammed Milhem—who have brought me through this journey with such care, compassion, and attentiveness. Not treated as a patient or a number, but as a person, as a family member of chondrosarcoma cancer.
The clinic nurses, receptionists, staff, the many X-ray technicians, lab, C scans, housekeeping, food services—the list could go on of all those I’ve crossed paths with through this journey. I can never repay or thank them enough for the excellent care given to me, my husband, and my family and friends.
Chondrosarcoma: Difficult to detect and diagnose
No one wants their story to start out with pain. But that is where my journey to chondrosarcoma begins.
I am a teacher in the gifted and talented program of a middle school. I was born out on the east coast, married, and now live outside Sac City, Iowa.
In 2012, I was struggling with back pain. I was 48 and enjoying adult volleyball, with many tournament wins under my belt. My doctor in Sac City thought I had a back problem. I believed it was age-related and that going for digs in volleyball was causing inflammation. So I took ibuprofen before activities to stay ahead of pain.
Then in 2013 my doctor suggested a cortisone shot to alleviate the pain. It didn’t work. Physical therapy was next, but that didn’t work. My husband, Bob, got fed up and called the doctor and said something else needed to be done. We were referred to Dr. Steven Meyer from Dakota Dunes.
‘Something was terribly wrong with me’
The day I volunteered to chaperone students to the rollerskating rink, pain overtook my body. As everyone boarded the bus to leave the rink, I was the last one left in the building, struggling to even get to the door. I was in tears with pain and embarrassment. Thankfully, the bus driver came back in and helped me get to the bus.
As we traveled back to school, with laughter, chattering, and enjoyment happening on the back of the bus, I was crying softly to myself. Every bump created pain. Something was terribly wrong with me. I decided to head to the ER.
After the same ER prep that would soon become routine for me, they sent me and my husband to another hospital to find the MRI truck and get tests done. Because it was a later appointment that night, they released me from the ER and sent me home. Bob had to CARRY me up the stairs and all the way to the sofa. I could no longer walk.
I had a long, sleepless night, hoping for answers at my appointment with Dr. Meyer.
A painful lesson: Get copies of your test results
I remember Dr. Meyer asking me, “Where is the pain?” I turned around and showed him my lower left back area. He asked if I had any tests. I said I had just had an MRI done.
That was when I found out that just because you have a test done at another hospital, those records and test results do not automatically get sent to your files. So I had nothing for him to look at. I was shocked, upset, disappointed, and didn’t understand.
Dr. Meyer ordered X-rays right then. He said the X-rays showed it was my hip, not my back. He said there was a “mass showing up” in my left pelvis bone.
I was dumbfounded. There was NO BUMP, NO BULGE. My body outside was showing NOTHING! Tears streamed down my face. In shock, I looked at an X-ray of a large cloudy mass.
He asked us where we wanted to go for further help. We decided on Iowa City. I am a HUGE Hawkeye fan, so in the back of my mind, more drives to Hawkeye country brought me comfort.
We were referred to Dr. Benjamin Miller for an appointment the next day. We headed to Iowa City the next day. The wheelchair became a necessity to get around the hallways and wings of University of Iowa Hospitals and Clinics.
My life is changed by a single word
The next day I was diagnosed as 1 in 1,400 in the United States to have chondrosarcoma cancer. I was told I was in Stage 3. The mass had deteriorated much of the left pelvis bone.
I had never heard the word chondrosarcoma, couldn’t pronounce or spell it. Yet this word will remain with me for the rest of my life.
Dr. Miller recommended getting me on crutches immediately and getting weight off that hip to prevent further damage. I chose epileptic crutches instead of armpit crutches so they wouldn’t be as stressful on my body.
We headed to oncology next and were told that it was an aggressive cancer. Our minds went whirling, both of us crying again.
Immediately, I was asked about being part of a clinical trial. I signed up, hoping my journey could help prevent someone else from going through what I would.
The surgery was scheduled four weeks later—Tuesday, May 6, 2014.
A lot happened in those four weeks. T-shirt fundraisers were done by my sister and my coworker Gene.
My life changed dramatically from normal to adjusting doing everything with crutches—sitting, showering, using the bathroom, standing, getting into and out of vehicles, to name a few. But I became an experienced “crutcher” by the time of my surgery.
Bob wrapped my crutches in black and yellow duct tape, allowing me to enjoy my new legs and rock my Hawkeye pride. That made it easier for others to accept me and approach me.
Surgery, and the road to recovery
Scared is an understatement. Thoughts of things going wrong raced through my mind and heart as I scanned the room to see the X-rays glowing on the wall, staff moving around everywhere. The anesthesiologist put the mask on and had me start counting.
I woke in the ICU with a nurse adjusting equipment and talking to me. My family was to my left but a blur. I heard the nurse tell them to let me rest and get supper.
When my family came back, my husband passed out beside my bed and was taken to another floor to be observed overnight. So family went back and forth between rooms.
I laid on a hospital bed on my back for several days, left leg and hip wrapped, drainage tubes from the hip area, catheter still in place. Daily blood draws first thing in the morning. Doctors, nurses, housecleaning, kitchen servers, other staff, visitors in and out all day in our room.
I was transported to rehabilitation in Des Moines, where I was told I would be there for around 21 days. Long story short, I worked hard, fought fevers, bedpans in bed, learned to readjust most every part of my life.
Nine days later, I proved I was strong and was ready to head home. I remember my last lap of proof with the walker around the track.
Arriving home, we were made aware of simple issues not thought about. The garage stairs leading into the house needed railings. The width of the doorways was too small for the wheelchair. We changed the bedroom layout to get me closer access to the bathroom. The furniture layout was moved around for wheelchair accessibility.
I was taking medicine at least three different times daily. My husband kept track, ordered refills, and many a day begged me to take my pills. An array of equipment was found or purchased to support the transition.
Chemo treatments begin
As we settled that first week at home, the phone call came. Dr. Miller’s office had next-day appointments, including with our oncologist, Dr. Mo Milhem.
The news from the pathologist came—two spots of dedifferentiated cancer forming. Dr. Miller said these WERE the worst of my cancer, and if they reached my lungs, very little could be done. Bob and I cried hard, hugging and trying to understand.
Dr. Mo instructed us that he would be giving us the strongest chemo he could, once a month for the next three months.
So my summer in 2014 was trips to Iowa City, hospital stays from Thursday to Sunday. I was filled with bags and bags of fluids to support the chemo in my veins and body. Friday and Saturday I received the chemo.
The first month my body became bloated, uncomfortable, body feeling heavy. The second month of chemo I was extremely nauseated. One medicine after another until they found something my body finally tolerated and helped.
All my hair fell out in July, eyebrows, head, nose, arms, eyelashes, legs. The third month was horrible chills and fevers, checking my temps every couple hours. If my temperature went over 101.7, I was to get myself into the ER to reduce my fever. I ended up at the ER many times.
Setbacks—and moving forward
Lots happened those summer months, shots after chemo, trips to the hospital for ER, outpatient, traveling three and a half hours each way every third week while still being in the hip/leg brace.
I couldn’t bend to get into our vehicles. We had issues with the brace as the ball started slipping out of the socket. Standing in the garage I could only drool on the floor with such pain. Bob immediately called an ambulance.
Upon arriving at the local ER, X-rays were taken, and Dr. Miller was notified immediately. He ordered me and my crippled body down to Iowa City for his care. They adjusted the brace, put a rod support down my leg.
I thought I could leave, only to find out my fevers were back again, and I was admitted again into the hospital. My immune system so low, I acquired fungus in my lungs.
A year later, the early part of August, I started noticing my hip was changing in size with a hump forming. I took pics and sent them to Dr. Miller. We learned infection had grown down to the bone and immediate surgery was needed to flush out all the infection.
I learned that as long as I have hardware in the pelvis, I’ll have infection. That’s when the infectious disease doctor became a part of my journey.
A PICC line was placed in my right arm, and for over a month I carried a bag of amoxicillin. All that a nurse would probably do, Bob and I did on our own—cleaning, changing, every little detail done.
Soon the numbers slowly started to lower, fevers finally started lowering, and the PICC line was removed.
I continue to use epileptic crutches daily, able to put a little weight on my hip. I am able to do most of my care, but I struggle with cooking, with holding and carrying and picking up things, with turning off light switches.
I have moments of frustration, occasional days in bed crying, wishing I could have my normal life back. I have sporadic pain in my hip, weak muscles in the left hamstring and calf, daily nerve pains in my foot that feel like your funny bone getting bumped.
I AM a survivor!
I AM a fighter. I continue to be strong-willed, encouraging others. I am daily supported and helped by Bob.
I look daily at my body and what is left of my left pelvis area, the huge scar—MY survivor scar—and I accept that I AM a survivor! I am able to drive. I believe my faith, strength, and determination come from my faith in God and His plan for me.
And so my journey continues now into “uncharted water,” as Dr. Miller calls it. Opening myself up to possibilities!